Predictors of in-hospital mortality among patients with status epilepticus in Lubumbashi, Democratic Republic of the Congo: A retrospective study
Main Article Content
Abstract
Objective: Status Epilepticus (SE) is a condition characterized by an epileptic seizure that persists long enough or recurs at sufficiently short intervals to create a fixed and lasting epileptic condition. The objective of this study was to determine the prevalence and to identify predictors of in-hospital death among SE patients in Lubumbashi, Democratic Republic of the Congo (DRC).
Methods: We conducted a retrospective study from January 2020 to December 2022.
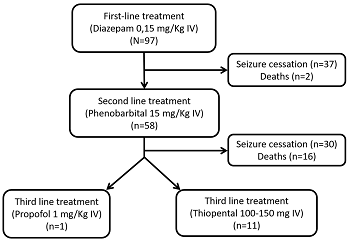
Results: Out of 3,006 patients admitted to the neurology department of the University Clinics of Lubumbashi, 97 presented with SE (i.e., a hospital prevalence of 3.23%). The mean age of the patients was 38.38±14.74 years, and men represented 77.3% of the cases. Epileptic patients represented 21.65% of the cases and 66.7% of them were on antiepileptic drugs (AEDs). Seizures were generalized in 72.16% of the patients. Seizures lasted 30 minutes or more in 50.52% of the cases. The most frequent etiologies were strokes, followed by central nervous system (CNS) infections. In-hospital mortality was 24.74% and the predictors of this mortality were CNS infections (adjusted OR = 22.34 [2.69-222.65]; p = 0.0006) and seizures lasting ≥ 30 minutes (adjusted OR = 10.98 [2.89-62.70]; p<0.0001).
Conclusion: SE is a major neurological emergency requiring early and multidisciplinary management to preserve the vital prognosis because, without treatment, SE causes important neurological complications and even death. The present study found a mortality of 24.74% which was associated with seizure duration of more than 30 minutes as well as with infectious etiologies.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
References
- Alolayan YS, McKinley K, Bhatia R, et al. Review and Updates on the Treatment of Refractory and Super Refractory Status Epilepticus. Journal of Clinical Medicine. 2021, 10(14): 3028. https://doi.org/10.3390/jcm10143028
- Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus – Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015, 56(10): 1515-1523. https://doi.org/10.1111/epi.13121
- Newton CR, Kariuki SM. Status epilepticus in sub‐Saharan Africa: New findings. Epilepsia. 2013, 54(s6): 50-53. https://doi.org/10.1111/epi.12277
- Cisse FA, Tassiou NR, Barry SD, et al. Évaluation de la prise en charge des états de mal épileptiques convulsifs en milieu tropical. Revue Neurologique. 2017, 173: S45. https://doi.org/10.1016/j.neurol.2017.01.023
- Leitinger M, Trinka E, Zimmermann G, et al. Epidemiology of status epilepticus in adults: Apples, pears, and oranges — A critical review. Epilepsy & Behavior. 2020, 103: 106720. https://doi.org/10.1016/j.yebeh.2019.106720
- Ngugi AK, Kariuki SM, Bottomley C, et al. Incidence of epilepsy. Neurology. 2011, 77(10): 1005-1012. https://doi.org/10.1212/wnl.0b013e31822cfc90
- Kariuki SM, Kakooza-Mwesige A, Wagner RG, et al. Prevalence and factors associated with convulsive status epilepticus in Africans with epilepsy. Neurology. 2015, 84(18): 1838-1845. https://doi.org/10.1212/wnl.0000000000001542
- Towne AR, Waterhouse EJ, Boggs JG, et al. Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000, 54(2): 340-340. https://doi.org/10.1212/wnl.54.2.340
- Dham BS, Hunter K, Rincon F. The Epidemiology of Status Epilepticus in the United States. Neurocritical Care. 2014, 20(3): 476-483. https://doi.org/10.1007/s12028-013-9935-x
- Ozdilek B, Midi I, Agan K, et al. Episodes of status epilepticus in young adults: Etiologic factors, subtypes, and outcomes. Epilepsy & Behavior. 2013, 27(2): 351-354. https://doi.org/10.1016/j.yebeh.2013.02.023
- Amare A, Zenebe G, Hammack J, et al. Status epilepticus: Clinical presentation, cause, outcome, and predictors of death in 119 Ethiopian patients. Epilepsia. 2008, 49(4): 600-607. https://doi.org/10.1111/j.1528-1167.2008.01556.x
- Scholtes FBJ, Renier WO, Meinardi H. Status epilepticus in children. Seizure. 1996, 5(3): 177-184. https://doi.org/10.1016/s1059-1311(96)80033-1
- Eriksson K, Koivikko M. Status epilepticus in children: aetiology, treatment, and outcome. Developmental Medicine & Child Neurology. 1997, 39(10): 652-658. https://doi.org/10.1111/j.1469-8749.1997.tb07358.x
- Poursadeghfard M, Hashemzehi Z, Ashjazadeh N. Status Epilepticus in Adults: A 6-Year Retrospective Study. Galen Medical Journal. 2014, 3(3): e200. https://doi.org/10.31661/gmj.v3i3.200
- Akyuz E, Polat AK, Eroglu E, et al. Revisiting the role of neurotransmitters in epilepsy: An updated review. Life Sciences. 2021, 265: 118826. https://doi.org/10.1016/j.lfs.2020.118826
- Hanada T. Ionotropic Glutamate Receptors in Epilepsy: A Review Focusing on AMPA and NMDA Receptors. Biomolecules. 2020, 10(3): 464. https://doi.org/10.3390/biom10030464
- Reddy Y, Balakrishna Y, Mubaiwa L. Convulsive status epilepticus in a quaternary hospital paediatric intensive care unit (PICU) in South Africa: An 8 year review. Seizure. 2017, 51: 55-60. https://doi.org/10.1016/j.seizure.2017.07.016
- Mbodj I, Ndiaye M, Sene F, et al. Prise en charge de l’état de mal épileptique dans les conditions de pays en développement. Neurophysiologie Clinique/Clinical Neurophysiology. 2000, 30(3): 165-169. https://doi.org/10.1016/s0987-7053(00)00203-3
- Moghaddasi M, Joodat R, Ataei E. Evaluation of Short-term Mortality of Status Epilepticus and Its Risk Factors. Journal of Epilepsy Research. 2015, 5(1): 13-16. https://doi.org/10.14581/jer.15003
- Langer JE, Fountain NB. A retrospective observational study of current treatment for generalized convulsive status epilepticus. Epilepsy & Behavior. 2014, 37: 95-99. https://doi.org/10.1016/j.yebeh.2014.06.008
- Lamine T, Moustapha N, Eva Sandrine KJ, et al. Assessment of State of Convulsive Child in Hospital National Children Albert Royer, Dakar. Clinical Pediatrics: Open Access. 2017, 02(01). https://doi.org/10.4172/2572-0775.1000116
- Nguefack S, Mbassi H D, Kouam M K, et al. Etiologies et évolution à court terme de l’état de mal convulsif inaugural du nourrisson et de l’enfant dans deux hôpitaux universitaires de Yaoundé (Cameroun). Health sciences and disease. 2016, 17(1). https://doi.org/10.5281/hsd.v17i1.568
- Thomas S, Cherian A. Status epilepticus. Annals of Indian Academy of Neurology. 2009, 12(3): 140. https://doi.org/10.4103/0972-2327.56312
- Lothman E. The biochemical basis and pathophysiology of status epilepticus. Neurology. 1990, 40(suppl 2): 13-23.
- Ramakrishnan KA, Levin M, Faust SN. Bacterial meningitis and brain abscess. Medicine. 2013, 41(12): 671-677. https://doi.org/10.1016/j.mpmed.2013.09.013
- Klein RS, Garber C, Howard N. Infectious immunity in the central nervous system and brain function. Nature Immunology. 2017, 18(2): 132-141. https://doi.org/10.1038/ni.3656
- Archibald LK, Quisling RG. Central Nervous System Infections. Textbook of Neurointensive Care. Published online 2013: 427-517. https://doi.org/10.1007/978-1-4471-5226-2_22
- Salimi H, Klein RS. Disruption of the Blood-Brain Barrier During Neuroinflammatory and Neuroinfectious Diseases. Neuroimmune Diseases. Published online 2019: 195-234. https://doi.org/10.1007/978-3-030-19515-1_7