Visual Conformity with One’s Affirmed Gender, or Blending In, and Its Relationship to Psychological Distress among Transgender Adults
Main Article Content
Abstract
Purpose: Very little research has examined the issue of visual conformity with one's affirmed gender (commonly referred to as "passing'') among transgender persons. This paper examines this phenomenon and its relationship to psychological distress in a sample of transgender adults.
Methods: Data from the 2015 U.S. National Transgender Survey were used to examine the relationship between visual conformity with one's gender-of-identity (dichotomous measure) and overall level of psychological distress (scale measure) in a sample of 26,649 transgender Americans aged 18 or older. Multivariate and structural equation analyses were preformed to examine the data.
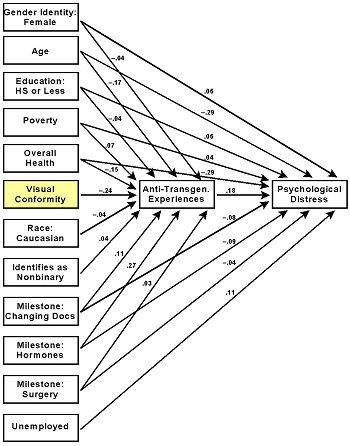
Results: 55% of the study participants reported attaining visual conformity with their affirmed gender. Visual conformity was related to psychological distress in bivariate analysis, but its effects were rendered statistically nonsignificant in a multivariate analysis. Structural equation analysis showed that visual conformity has a significant, inverse impact upon the number of anti-transgender experiences people incur and those experiences, in turn, are related directly and strongly to psychological distress.
Conclusions: Visual conformity with one's gender-of-identity is an important consideration when trying to understand the extent to which transgender persons experience psychological distress. Its effects operate indirectly, though, principally through their impact upon the number of anti-transgender acts of discrimination, harassment, and violence that people incurred.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
References
- Anderson AD, Irwin JA, Brown AM, et al. “Your Picture Looks the Same as My Picture”: An Examination of Passing in Transgender Communities. Gender Issues. 2019, 37(1): 44-60. https://doi.org/10.1007/s12147-019-09239-x
- Marques AC. Displaying Gender: Transgender People’s Strategies in Everyday Life. Symbolic Interaction. 2019, 42(2): 202-228. https://doi.org/10.1002/symb.412
- To M, Zhang Q, Bradlyn A, et al. Visual Conformity with Affirmed Gender or “Passing”: Its Distribution and Association with Depression and Anxiety in a Cohort of Transgender People. The Journal of Sexual Medicine. 2020, 17(10): 2084-2092. https://doi.org/10.1016/j.jsxm.2020.07.019
- Parr NJ, Howe BG. Factors associated with frequency of gender identity nonaffirmation microaggressions among transgender persons. Culture, Health & Sexuality. 2020, 23(8): 1094-1110. https://doi.org/10.1080/13691058.2020.1755454
- Kattari SK, Hasche L. Differences Across Age Groups in Transgender and Gender Non-Conforming People’s Experiences of Health Care Discrimination, Harassment, and Victimization. Journal of Aging and Health. 2015, 28(2): 285-306. https://doi.org/10.1177/0898264315590228
- Rood BA, Maroney MR, Puckett JA, et al. Identity concealment in transgender adults: A qualitative assessment of minority stress and gender affirmation. American Journal of Orthopsychiatry. 2017, 87(6): 704-713. https://doi.org/10.1037/ort0000303
- Kcomt L, Evans-Polce RJ, Veliz PT, et al. Use of Cigarettes and E-Cigarettes/Vaping Among Transgender People: Results From the 2015 U.S. Transgender Survey. American Journal of Preventive Medicine. 2020, 59(4): 538-547. https://doi.org/10.1016/j.amepre.2020.03.027
- Connolly D, Gilchrist G. Prevalence and correlates of substance use among transgender adults: A systematic review. Addictive Behaviors. 2020, 111: 106544. https://doi.org/10.1016/j.addbeh.2020.106544
- James SE, Herman JL, Rankin S, et al. The report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality, 2016.
- Garcia J, Gustavson AR. The science of self-report. 1997. https://www.psychologicalscience.org
- Zajacova A, Dowd JB. Reliability of Self-rated Health in US Adults. American Journal of Epidemiology. 2011, 174(8): 977-983. https://doi.org/10.1093/aje/kwr204
- Arrow K, Resnik P, Michel H, et al. Evaluating the Use of Online Self-Report Questionnaires as Clinically Valid Mental Health Monitoring Tools in the Clinical Whitespace. Psychiatric Quarterly. 2023, 94(2): 221-231. https://doi.org/10.1007/s11126-023-10022-1
- KESSLER RC, ANDREWS G, COLPE LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002, 32(6): 959-976. https://doi.org/10.1017/s0033291702006074
- Prochaska JJ, Sung H, Max W, et al. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research. 2012, 21(2): 88-97. https://doi.org/10.1002/mpr.1349
- Klein H, Washington TA. Transition Milestones and Psychological Distress in Transgender Adults. Urban Social Work. 2023, 7(1): 66-84. https://doi.org/10.1891/usw-2022-0016
- Klein H, Washington TA. Transition Milestones, Psychological Distress, and Suicidal Ideation Among Transgender Adults: A Structural Equation Analysis. OMEGA - Journal of Death and Dying. Published online December 8, 2023. https://doi.org/10.1177/00302228231221308
- Cohen J. Statistical power analysis for the behavioral sciences (second edition). Routledge: New York, 1988.
- Dorey FJ. In Brief: Statistics in Brief: Statistical Power: What Is It and When Should It Be Used? Clinical Orthopaedics & Related Research. 2011, 469(2): 619-620. https://doi.org/10.1007/s11999-010-1435-0
- Szumilas M. Explaining odds ratios. Journal of the American Academy of Child and Adolescent Psychiatry. 2010, 19: 227-229.
- Alavi M, Visentin DC, Thapa DK, et al. Chi‐square for model fit in confirmatory factor analysis. Journal of Advanced Nursing. 2020, 76(9): 2209-2211. https://doi.org/10.1111/jan.14399
- Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods of psychological research online. 2003, 8(2): 23-74.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999, 6(1): 1-55. https://doi.org/10.1080/10705519909540118
- Van Laar S, Braeken J. Understanding the Comparative Fit Index: It's All about the Base!. Practical Assessment, Research & Evaluation. 2021, 26: 26.
- Pavlov G, Maydeu-Olivares A, Shi D. Using the Standardized Root Mean Squared Residual (SRMR) to Assess Exact Fit in Structural Equation Models. Educational and Psychological Measurement. 2020, 81(1): 110-130. https://doi.org/10.1177/0013164420926231
- Gómez-Gil E, Zubiaurre-Elorza L, Esteva I, et al. Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology. 2012, 37(5): 662-670. https://doi.org/10.1016/j.psyneuen.2011.08.010
- Heylens G, Verroken C, De Cock S, et al. Effects of Different Steps in Gender Reassignment Therapy on Psychopathology: A Prospective Study of Persons with a Gender Identity Disorder. The Journal of Sexual Medicine. 2014, 11(1): 119-126. https://doi.org/10.1111/jsm.12363
- Gorin-Lazard A, Baumstarck K, Boyer L, et al. Is Hormonal Therapy Associated with Better Quality of Life in Transsexuals? A Cross-Sectional Study. The Journal of Sexual Medicine. 2012, 9(2): 531-541. https://doi.org/10.1111/j.1743-6109.2011.02564.x
- Gorin-Lazard A, Baumstarck K, Boyer L, et al. Hormonal Therapy Is Associated With Better Self-esteem, Mood, and Quality of Life in Transsexuals. Journal of Nervous & Mental Disease. 2013, 201(11): 996-1000. https://doi.org/10.1097/nmd.0000000000000046
- Eisenberg E, Zervoulis K. All flowers bloom differently: an interpretative phenomenological analysis of the experiences of adult transgender women. Psychology & Sexuality. 2019, 11(1-2): 120-134. https://doi.org/10.1080/19419899.2019.1661278
- Fein LA, Salgado CJ, Alvarez CV, et al. Transitioning Transgender: Investigating the Important Aspects of the Transition: A Brief Report. International Journal of Sexual Health. 2016, 29(1): 80-88. https://doi.org/10.1080/19317611.2016.1227013
- Moody C, Fuks N, Peláez S, et al. “Without this, I would for sure already be dead”: A qualitative inquiry regarding suicide protective factors among trans adults. Psychology of Sexual Orientation and Gender Diversity. 2015, 2(3): 266-280. https://doi.org/10.1037/sgd0000130
- Owen-Smith AA, Gerth J, Sineath RC, et al. Association Between Gender Confirmation Treatments and Perceived Gender Congruence, Body Image Satisfaction, and Mental Health in a Cohort of Transgender Individuals. The Journal of Sexual Medicine. 2018, 15(4): 591-600. https://doi.org/10.1016/j.jsxm.2018.01.017
- McNichols CHL, O’Brien-Coon D, Fischer B. Patient-reported satisfaction and quality of life after trans male gender affirming surgery. International Journal of Transgender Health. 2020, 21(4): 410-417. https://doi.org/10.1080/26895269.2020.1775159
- Davis SA, St. Amand C. Effects of Testosterone Treatment and Chest Reconstruction Surgery on Mental Health and Sexuality in Female-To-Male Transgender People. International Journal of Sexual Health. 2014, 26(2): 113-128. https://doi.org/10.1080/19317611.2013.833152
- Staples JM, Bird ER, Gregg JJ, et al. Improving the Gender-Affirmation Process for Transgender and Gender-Nonconforming Individuals: Associations Among Time Since Transition Began, Body Satisfaction, and Sexual Distress. The Journal of Sex Research. 2019, 57(3): 375-383. https://doi.org/10.1080/00224499.2019.1617829
- van de Grift TC, Elaut E, Cerwenka SC, et al. Effects of Medical Interventions on Gender Dysphoria and Body Image: A Follow-Up Study. Psychosomatic Medicine. 2017, 79(7): 815-823. https://doi.org/10.1097/psy.0000000000000465
- Transgender Institute (2023a). Feminine immersion program. https://transinstitute.org
- Transgender Institute (2023b). Men’s program. https://transinstitute.org
- Duke Health (2022). Gender-affirming treatment and transition care. https://www.dukehealth.org
- Trans Lifeline (2023). A binding guide for all genders and gender expressions. https://translifeline.org
- Oregon Health and Science University (2023). Transgender health program patient education and events. https://www.ohsu.edu
- DeFilippis JN. “What About the Rest of Us?” An Overview of LGBT Poverty Issues and a Call to Action. Journal of Progressive Human Services. 2016, 27(3): 143-174. https://doi.org/10.1080/10428232.2016.1198673
- Gonzales G, Henning-Smith C. Barriers to care among transgender and gender nonconforming adults. The Milbank Quarterly. 2017, 95(4): 726-748. https://doi.org/10.1111/1468-0009.12297
- Kcomt L, Gorey KM, Barrett BJ, et al. Unmet Healthcare Need Due to Cost Concerns among U.S. Transgender and Gender-Expansive Adults: Results from a National Survey. Health & Social Work. 2021, 46(4): 250-259. https://doi.org/10.1093/hsw/hlab029
- Kilikita J. As a trans woman, I understand the pressure to pass. But it’s holding us back. 2021. https://www.refinery29.com
- WCMU (2017). What does it mean to ‘pass’ as a transgender person? https://radio.wcmu.org
- Tannehill B. For many trans people, not passing is not an option. 2018. https://slate.com